OCD Help From a Muslim Therapist
About Aisha Chaudhry
Dr. Aisha Chaudhry is an Aalimah and Muslim Therapist. She specializes in trauma which often looks like depression, anxiety including OCD, intrusive thoughts, health anxiety, and panic. She has a special interest in helping clients learn how to calm the body through a combination of neural informed therapies, Internal Family Systems, CBT, and Exposure-Response Prevention. For clients looking for integrated therapy, a holistic approach is available.
Table of Contents
OCD Help from a Muslim Therapist
The information contained herein is to offer a comprehensive overview of OCD (not for treatment or diagnosis) with special emphasis on what OCD often looks like in some of the Muslim populations. It is important to get treatment from a Muslim therapist, particularly, one who has studied Islam and who knows the Islamic rulings surrounding the issues clients seek treatment for. The reasons are two-fold:
- Therapeutic Alliance: It is important for the client to develop a good therapeutic relationship with the therapist. This can only happen if the client feels safe enough to discuss matters that they feel embarrassed about or fear they may be judged negatively due to them. Sometimes the themes related to the obsessions are very difficult to communicate to anyone, which is one of the reasons for lack of seeking care at all. Additionally, to help the client feel comfortable with the treatment plan, the therapist should be well-versed in Islamic rulings because individuals with OCD tend to have a lot of doubts and fears that perhaps they are sinning or will be punished. The topics that often come up for Muslim populations are often related to what they value most, and often that is religious-oriented themes and contamination issues related to food and purity. Of course, other themes are present as well but more likely than not clients will have more than one theme present.
- Accurate Diagnosing. What OCD looks like among the Muslim population can significantly vary from other populations, which can cause OCD to either go undiagnosed or even misdiagnosed. The obsessions and compulsions related to OCD are typically focused on what an individual values the most. Sometimes Muslims may seem to be more religious, have more piety (taqwa) or engage in more rituals. Behaviors may or may not reflect an accurate depiction because the practice of Islam may seem more or less obsessive in one particular area over another. A properly trained clinician would be able to decipher between content and process, which is important in diagnosing and treating.
What is OCD?
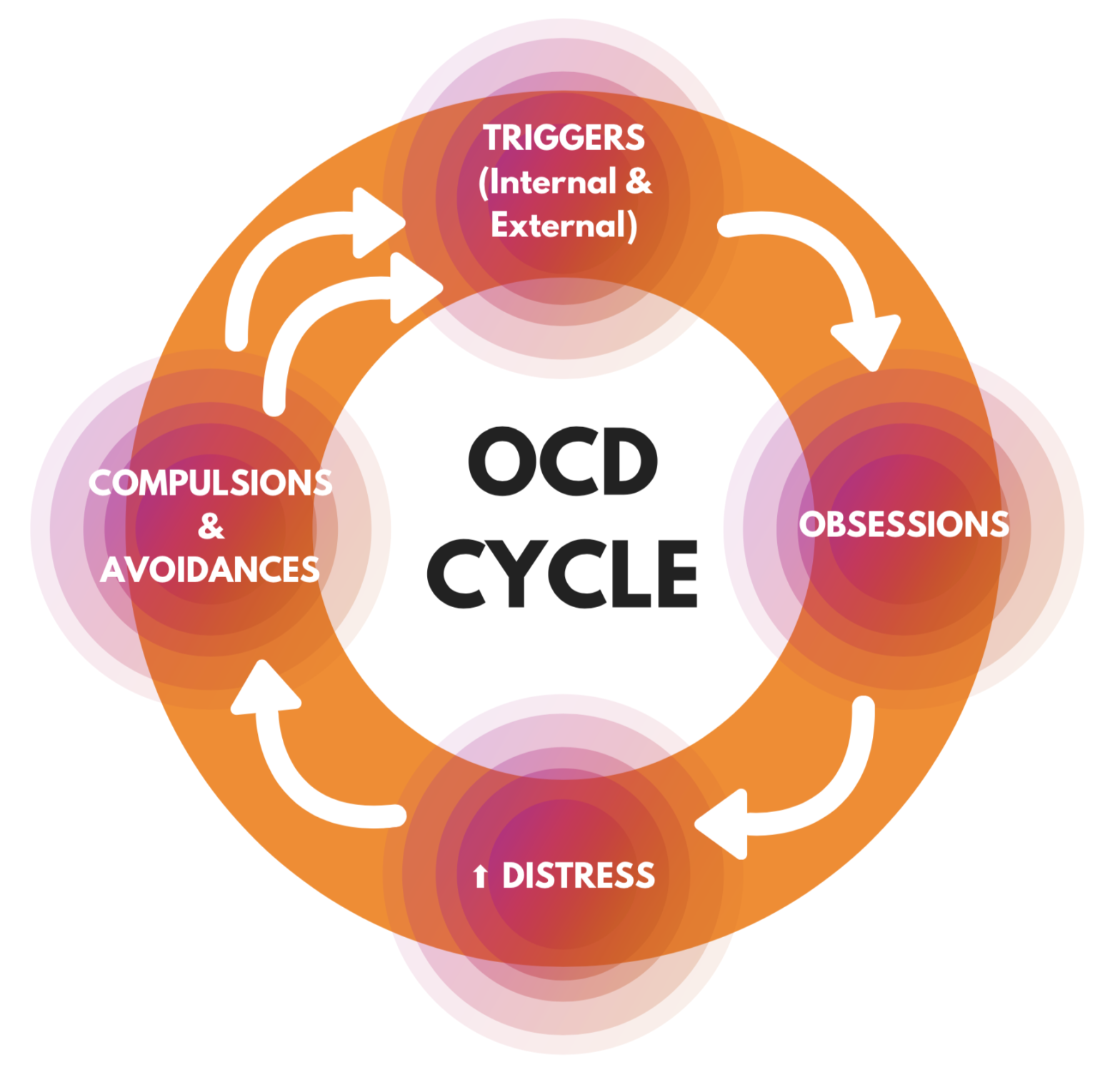
Obsessive-compulsive disorder (OCD) is a disorder in which people have recurring, unwanted thoughts, ideas, images, or sensations (obsessions) that make them feel driven to do something repetitively (compulsions). Repetitive behaviors, such as hand washing, checking on things, or cleaning, can significantly interfere with a person’s daily activities and social interactions.
It is very normal for distressing, repetitive thoughts to enter anyone’s mind, at any time, however, the difference is that they typically don’t remain in the mind for too long and they do not cause distress to the point of disrupting daily life.
Individuals who suffer from OCD have thoughts that are persistent and as a result, they begin to engage in rigid behaviors; they often will have the family engaging in their behaviors as well because it’s either easier to deal with if they just comply. When a person suffers from OCD, the distress is so great that they find themselves consumed for sometimes hours in a day or many hours over the course of a day trying to gain relief or satisfaction from the distressing thoughts or images. They may feel not performing behaviors (rituals) is nearly not an option or if they do manage to ignore the thoughts and move on, they often suffer through it. For some individuals, they do not engage in an external behavior or perhaps they are unaware of that external behavior. For example, if a distressing, intrusive thought comes, they may mentally negate it – while showing nothing externally to witness. For this reason, individuals may suffer for quite a long time without anyone knowing that anything is actually occurring. Sometimes individuals suffering aren’t aware at all that they are suffering. They may have strong beliefs that what they are doing is correct and may even see it as being the best version of themselves.
The Think-About:
Struggling with OCD can feel like being stuck on a roundabout where some cars are able to exit the roundabout but individuals with OCD cannot without great distress. They might look at the exits of the roundabout and wish to exit, but they just keep circling around and around the center, which I call the theme. It feels like a loop, and the sufferer really struggles to get off. I call this roundabout a “think-about” because the individual keeps thinking and thinking and they get enough reassurances and satisfaction and get off, but then after a short period of time, they find themselves right back on that same think-about.
Getting help with OCD from a Muslim therapist can be helpful because we can learn how to get off of this negative thinkabout and onto a healthier one which incorporates moderate views of Islam and incorporates other attributes of Allah in a more balanced way. Allah swt isn’t just the one who will punish us. He is so many other things, like the one who has mercy, provides, nourishes, and loves us. Getting help with OCD from a Muslim therapist will help you to balance these views in sha Allah.
What are Obsessions?
Obsessions are recurrent and persistent thoughts, impulses, or images that cause distressing emotions such as anxiety or disgust. Many people with OCD recognize that the thoughts, impulses, or images are a product of their minds and are excessive or unreasonable. However, the distress caused by these intrusive thoughts cannot be resolved by logic or reasoning. Most people with OCD try to ease the distress of the obsessions with compulsions, ignore or suppress the obsessions, or distract themselves with other activities.
A Few Broad Areas of Obsessions:
- Religious or moral scrupulosity
- Relationship obsessions (current or previous)
- Obsessional jealousy
- Fear of making a mistake while reading the Quran
- Uncertainty about not being clean (for prayers, reading, etc)
- Uncertainty of completeness or correctness
- Fear of not saying or doing something just right
- Not saying a particular dua or phrase will be cause harm
- Fear of getting contaminated by people or the environment
- Fear of food getting contaminated
- Obsessive worries about food being halal or haram
- Disturbing sexual and/or violent thoughts or images
- Fear of harming self or someone else (stabbing, killing, running over, punching, kicking)
- Excessively doubting oneself or other’s intentions about anything
- Fear of blurting out obscenities or insults
- Extreme concern with order, symmetry, or precision
- Recurrent intrusive thoughts of sounds, images, words, or numbers
- Fear of losing or discarding something important
- Constant thoughts about a particular part of the body
- Excessive concern with having an illness
- Excessive worry about breaking rules
- Repeating numbers or phrases
What Individuals With OCD Say
OCD can appear over one specific area or many areas of one’s life. Below are just examples of what clients might say to give you an idea of what an obsessive thought or fear might sound like. Please keep in mind that everyone has the same thoughts, but an individual with OCD struggles with those thoughts believing they are real or valid to the point of engaging in other behaviors to calm down that fear or thought (known as a compulsion or ritual. We will talk more about that coming up.) OCD help from a Muslim therapist will be beneficial because all of my clients are Muslims, and I have the benefit of knowing exactly where some of the issues are religiously, culturally, and interpersonally.
Clients often say things like:
- I have blasphemous thoughts about Allah or the Prophet (saw) and I may go to Hell.
- I don’t think Allah will forgive me.
- If I don’t pray just right I will go to Hell, and I don’t want to be sinful.
- I think I need to do everything 3 times or I’ll be sinful or not accepted.
- I am never really sure if I did things right
- I don’t know if I have wudhu or ghusl
- Maybe I didn’t clean myself properly
- Maybe I made a mistake in reading Quran and I should start over
- Does my spouse or family really love me?
- Do I really love my spouse or family?
- Did I marry the right person or is this the right person to marry?
- Maybe I need to fix this a bit more
- I need a lot of reassurance from others or my spouse. I am not sure how others really feel.
- I have too many thoughts and sometimes I just want to drown them out
- I have disturbing, violent thoughts or images
- I have intrusive sexual, sexually aggressive, or seemingly inappropriate thoughts or images
- I have a lot of very embarrassing thoughts and sensations happening in my body
- I fear I might be homosexual
- I am afraid I might hurt someone or myself
- I feel like I am never saying my prayers correctly
- I never feel sure I’ve cleaned myself properly
- I am not sure if I have wudhu
- I check and often recheck things a lot to make sure it’s off, a person is still alive, or a person is unharmed
- I have thoughts or images of stabbing someone, running over someone, or pushing, kicking, punching someone
- I think someone will get hurt or ill and it’ll be my fault
- I need to make sure everyone is safe and that I have exerted in making sure everyone’s safe because if someone were to get harmed or sick, it will be my fault and I can’t bear that
- I need to make sure there are no germs, residues of chemicals, or contaminants that might make me or someone else ill or poisoned
- I count, line up, repeat, re-read, make lists, make things symmetrical, keep things in a certain way,
- I am sure I’ve committed sins that Allah won’t forgive
- Maybe I didn’t ask for forgiveness properly or sincerely enough
- Maybe because of these thoughts I am going to be punished
- Maybe my spouse is in love with someone else or not in love with me
- Maybe my spouse wishes he had married someone else
- What if I made a mistake and now my children and their future is at stake
- Do I owe money to people?
- Did I steal something because of a coupon, discount, or misunderstanding of a sale or promotion?
- Did I pull one over on someone?
- Did I cheat on my taxes?
- Is this part of my face symmetrical compared with the other
- I just need to fix the nails or skins on my fingers or toes (leading to biting, picking, with and without tools)
- Maybe this hair is not matching with the other (leading to hair pulling or perhaps a part of safety-seeking)
- I need to tell someone I did something wrong or broke a rule
Don't Believe Everything You Think
Just because you think it or fear it does not make it true. Sometimes the brain has a stubborn desire to hold on to a particular belief, particular if the stakes seem high. And sometimes it’s as though images of random frightening or repulsive things flash through the mind. What do you say about yourself when these thoughts and images come? It is hard to bear, so we go into overdrive to stop it all.
We will work fervently to ‘make sure’ something doesn’t happen or that we are not bad or sinful.
Those inner thoughts can feel like a bully or the voice of an inner critic. Aisha can help you learn how to take charge of your thoughts instead of thoughts taking charge of you, your life, and your family’s life.
About Compulsions
Compulsions are also called rituals that of usually performed in order to reduce distress related to an obsession. Compulsions are often repeated either by certain outward actions or mentally. Compulsions can either be directly related or unrelated to an obsession. These compulsions can take up a significant amount of time in a person’s day, resulting in other consequences like other disorders or interruption of functioning at work, school, social, or other areas of life.
Compulsions look like: checking, seeking reassuring, redoing, rereading, making sure, getting things ‘just’ right or balanced, trying to undo what has been done, negating, and any others. OCD is unique and what it looks like in a sufferer’s life is unique. But, the treatment for all will be the same. Getting help with OCD from a Muslim therapist will be beneficial because as Muslims, we know what rituals should look like in our deen – not the ones we create ourselves.
Common Examples of Compulsions:
- Repeating ablutions (wudhu) due to feelings of incompleteness, incorrectness, or some defect in it
- Doubt if one still has ablution (wudhu) to the point of that uncertainty causing them to repeat it
- Repeating watching of body or things, not being sure a proper shower (ghusl) has been completed, which compels a person to repeat the ghusl or complete the ghusl in a certain way “to be sure”
- Repeating prayers (salah) or doing sajda sahw unnecessarily
- Not being certain where one is prayers, which is not due to a neurological memory issue, so one might repeat the prayer or a part of it
- Doubting if one recited the Quran correctly or not and then repeating the verses or starting all over
- Repeating thikr or tasbih because you think you didn’t do it correctly or the right number of times and probably you’ve assigned a certain methodology or routine to the thikr that should be kept so you repeat it until it is just like you feel it should be
- Thinking that something might have dropped into the food which is forbidden (haram) or makrooh (disliked) and that compels the person to throw the food away and start fresh
- Doubting ingredients of a food or drink product although sound opinions are given which compels them to not purchase that product or consume it
- Excessive or ritualized hand washing, showering, brushing teeth, or toileting
- Repeated cleaning of household objects
- Ordering or arranging things in a particular way
- Repeatedly checking locks, switches, or appliances
- Creating lists upon lists so as to not forget or to make sure everything is listed or organized etc
- Making sure mistakes are not made and even apologizing just in case
- Constantly seeking approval or reassurance
- Repeatedly counting to a certain number
- Picking skin, biting nails, pulling out hair
- Drumming, tapping, making throaty sounds
- Making sure one part of the body does not contaminate the other part
- Making many doctor appointments or getting a lot of labs to make sure there is nothing wrong
- Research or googling different topics to make sure of the right or complete information, complete
- Repeatedly asking or inquiring in different ways to make sure the person understands the question correctly so that the wrong answer or results don’t come
- Getting up or turning toward the same number of times
- Getting divorced or moving out because of relationship obsessions to prevent the spouse from getting hurt, contaminated, poisoned, or otherwise ill.
- Seeking reassurance by spying (checking) spouse’s clothing, spouse’s email, browsing history, video watch history, social media accounts, or popping in at work etc
- Saying a particular duaa or verse of Quran with the conviction that if it is not said then someone will get hurt and perhaps blameworthy.
- Keeping a particular routine to ‘ensure’ nothing harmful comes with the conviction that if it’s not kept something bad will happen and perhaps blameworthy
- Doing different things to block or drown out sounds, images, or thoughts of any kind
Piety or OCD?
I do wish there was a way to definitely write down a checklist of is it piety or OCD. One issue is that there is a narration that basically in part says that sin is that thing that causes unease. (reference). On the other hand, Allah swt does not put on us more than we can bear, nor does He encourage excessive, rigid, or polarized thinking or behaviors.
“Abu Hurairah (ra) said; His companion came to him and said; Messenger of Allah (saw)! We have thoughts that we cannot dare talk about and we do not like that we have them or talk about them. He said: Have you experienced that? They replied: yes. He said: that is clear faith.” [Abu-Dawood: 5111].
For this reason, we have to take the whole person into consideration along with the thought and behavior processes. Getting help with OCD from a Muslim therapist will help because as Muslims, we can decipher between excessiveness, rigidity, and piety.
Rigidity often shows up in many areas of life, and with rigidity comes intolerance of oneself and others and their behaviors as well as other emotions like anger, outbursts, overwhelm, despair, and others.
In order to differentiate if a thought-behavioral pattern is being kept out of piety or if perhaps it is excessive due to OCD, we need to examine the cycle in more detail. Most likely you will need help from a qualified therapist to differentiate. If you are reading through this and you’re not sure, reach out.
Please keep in mind, that I usually get a lot of background information and then analyze it in totality to help you determine if you are a very pious person or if you are unfairly excessive in one area. I absolutely do not judge and wholeheartedly invite you to explore this. Understanding OCD often needs help.
- When you have the thought, how distressing is it? Does your mind try to write one outcome and ignore perspectives and possibilities?
- When you don’t engage in compulsions or rituals, what do you do or how do you cope?
- Are you engaging in safety behaviors such as avoiding, seeking reassurance, checking, repeating, etc? Ask yourself what do you do as a result of these thoughts?
- Are people at work, school, family, or social domains noticing something may not be ok or perhaps suggesting you should talk to someone?
- Are you asking other people to engage in your safety behaviors or rituals (to make sure everything will be ok)?
- Do you spend a lot of time trying to get through the distressing thoughts, images, or behavior?
- Are you feeling negative, disempowering emotions as a result of the thoughts, images, or behaviors?
- Would you say that you are equally pious in other areas of your life except for these couple of things? For example, a person does not eat halal, zabiha food regularly or doesn’t mind that much but on the other hand struggle with prayers or wudhu and is overly meticulous in comparison.
- Are others feeling it is really difficult to live and be around you?
- Ask yourself what will happen if you do not engage in that safety, ritualistic behavior. What comes up for you?
Diagnosing OCD
To diagnose OCD, I use the criteria specified by the American Psychiatric Association (APA). Additionally, I use one or more assessment instruments to create a baseline of symptoms and their severity. This helps us know where we are starting so that we know if we are progressing. However, as a Muslim therapist who has experience in treating OCD, I will look at the totality of a person in relation to religious practices. Not all clinicians will know without lengthy explanations on what would be considered excessive or creating a hardship for oneself.
The criteria is as follows:
Diagnostic Criteria – 300 3 (F42)
A. Presence of obsessions, compulsions, or both:
Obsessions are defined by (1) and (2):
- Recurrent and persistent thoughts, urges, or images that are experienced, at some time during the disturbance, as intrusive and unwanted, and that in most individuals cause marked anxiety or distress.
- The individual attempts to ignore or suppress such thoughts, urges, or images, or to neutralize hem with some other thought or action (i.e., by performing a compulsion).
Compulsions are defined by (1) and (2):
- Repetitive behaviors (e.g., hand washing, ordering, checking) or mental acts (e.g., praying, counting, repeating words silently) that the individual feels driven to perform in response to an obsession or according to rules that must be applied rigidly.
- The behaviors or mental acts are aimed at preventing or reducing anxiety or distress, or preventing some dreaded event or situation; however, these behaviors or mental acts are not connected in a realistic way with what they are designed to neutralize or prevent, or are clearly excessive.
B. The obsessions or compulsions are time-consuming (e.g., take more than 1 hour per day) or cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
C. The obsessive-compulsive symptoms are not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition.
D. The disturbance is not better explained by the symptoms of another mental disorder (e.g., excessive worries, as in generalized anxiety disorder; preoccupation with appearance, as in body dysmorphic disorder; difficulty discarding or parting with possessions, as in hoarding disorder; hair pulling, as in trichotillomania [hair-pulling disorder]; skin picking, as in excoriation [skin-picking] disorder; stereotypies, as in stereotypic movement disorder; ritualized eating behavior, as in eating disorders; preoccupation with substances or gambling, as in substance-related and addictive disorders; preoccupation with having an illness, as in illness anxiety disorder; sexual urges or fantasies, as in paraphilic disorders; impulses, as in disruptive, impulse-control, and conduct disorders; guilty ruminations, as in major depressive disorder; thought insertion or delusional preoccupations, as in schizophrenia spectrum and other psychotic disorders; or repetitive patterns of behavior, as in autism spectrum disorder).
To Be Specified:
- With good or fair insight: The individual recognizes that the obsessive-compulsive disorder beliefs are definitely or probably not true or that they may or may not be true.
- With poor insight: The individual thinks the obsessive-compulsive disorder beliefs are probably true.
- With absent insight/delusional beliefs: the individual is completely convinced that the obsessive-compulsive disorders beliefs are true.
- Tic-related: The individual has a current or past history or a tic disorder.
Treating OCD
Clients with OCD who seek treatment will often experience improvements in their quality of life across all domains. For example, people who were previously late, lacking in focus, losing relationships, avoiding events, struggling in relationships etc may notice they improve their functioning and are able to reengage in areas of life they value and improve relationships with people and relationships to ideologies that often help them even improve their spirituality and relationship with Allah swt.
Several types of therapies may be used to help clients with OCD. As a Muslim therapist dealing with Muslim clients, per my client’s comfort levels, I offer an integrated therapy helping them with Islamic principles and values that most find liberating. Please note that clients absolutely have the option of electing therapy without Islamic principles and values.
Cognitive behavioral therapy (CBT) is a form of psychological treatment that has been demonstrated to be effective for a range of problems including depression, anxiety disorders, alcohol and drug use problems, marital problems, eating disorders, and severe mental illness. Numerous research studies suggest that CBT leads to significant improvement in functioning and quality of life. In many studies, CBT has been demonstrated to be as effective as, or more effective than, other forms of psychological therapy or psychiatric medications.
There are many types of modalities or techniques used in CBT, but the technique used to treat Anxiety and Anxiety Spectrum Disorders like OCD among others is Exposure-Response Prevention (ERP). ERP is the gold standard treatment model and is excellent when enhanced or integrated with other therapies like Mindfulness, which includes Acceptance and Commitment Therapy (ACT). Regardless of the integration of other therapies into the mainframe treatment, ERP must be a part of the foundational therapy. The basic principles of ERP include the following:
- Obsessions, Compulsions, triggers, and safety behaviors are identified and ranked in terms of distress.
- Clients will be exposed to feared situations or images related to their obsessions which will elicit anxiety.
- Clients are instructed to avoid the compulsive behaviors, rituals, and safety behaviors (hence response prevention part of the treatment name).
- The client must stay exposed to the anxiety provoking situation, while witnessing that nothing terrible is happening as a result of not trying to control, prevent, or alter the feared outcome.
- The mind and body will learn that thoughts are just thoughts and not necessarily reality, which helps the nervous system and mind develop a healthier thought-response pattern.
- Anxiety due to the specified trigger will shift as exposures are repeated and no compulsions, rituals, or safety behaviors are engaged in.
Clients will learn that they can cope without relying on trying to alter, change, or control circumstances and that whatever comes up can be dealt with without engaging in those compulsions, rituals, or safety behaviors. Even if anxiety does come around it, it can be better managed.
A class of medications known as selective serotonin reuptake inhibitors (SSRIs), typically used to treat depression, can also be effective in the treatment of OCD. The SSRI dosage used to treat OCD is commonly higher than that used to treat depression. Clients who do not respond to one SSRI medication sometimes respond to another. Other psychiatric medications can also be effective. Noticeable benefit usually takes six to twelve weeks.
Clients with mild to moderate OCD symptoms are typically treated with either CBT or medication depending on patient preference, the client’s cognitive abilities and level of insight, the presence or absence of associated psychiatric conditions, and treatment availability. It is recommended that patients with severe OCD symptoms receive both CBT and medication.
Disclaimer: I am not recommending you take a medication or remove your current medication. Please talk to your prescriber to see if the medications are right for you.
- 7 out of 10 people will likely see a reduction of symptoms when taking medications.
- A higher dose is often necessary before some medications start working for OCD.
- Taking Benzodiazepines like Xanax can become a compulsion. Your brain may learn that the only way to reduce anxiety is to take this type of medication.
- Medication and treatment together can often make a big difference in reducing symptoms of OCD and anxiety.
Medications listed on IOCDF.org
- fluvoxamine (Luvox®) – up to 300 mg/day
- fluoxetine (Prozac®) – 40-80 mg/day
- sertraline (Zoloft®) – up to 200 mg/day
- paroxetine (Paxil®) – 40-60 mg/day
- citalopram (Celexa®) – up to 40 mg/day
- clomipramine (Anafranil®) – up to 250 mg/day
- escitalopram (Lexapro®) – up to 40 mg/day
- venlafaxine (Effexor®) – up to 375 mg/day
Some Psychiatrists choose to add what’s called an atypical antipsychotic medication if they are struggling to do treatment effectively. https://iocdf.org/about-ocd/ocd-treatment/meds/
NOTE: I do not prescribe medication, but I do request clients who are finding treatment too difficult due to the severity to seek help from a psychiatrist for medication suitable while continuing therapy together. My preference as a therapist is to try to improve on your own before seeking medication.
Neurosurgical treatment (e.g., deep brain stimulation, anterior capsulotomy) in refractory cases is sometimes also considered for treatment.
Deep brain stimulation has gained popularity in treating people with severe OCD that is not responding to other treatments. Some studies show that anterior capsulotomy, a surgical procedure, can also be effective but it is underused due to historical prejudice rather than lack of clinical effectiveness.
In people with OCD who live with family or caregivers, enlisting the support of caregivers to help with exposure practice at home is recommended. I often encourage individuals to have a buddy in order to help make sure they do not engage in safety behaviors as well as to instruct them not to reassure by educating them about these processes.
It is important for family members and friends to not allow themselves and their routines be changed due to OCD. Sometimes individuals with OCD will create a routine or habits in the home that supports their level of comfort and this can be extremely disrupting to others.
It is also important for family members not to reassure or validate thoughts a person with OCD has related to their obsessions. For example, if a person with OCD asks a spouse, “Do you really love me?” The spouse should not feel the need to reassure the person of their love. While this seems harsh if a person really needs that reassurance, maybe there is another issue with the relationship. An individual with OCD does not have any reason to ‘doubt’ love for example so reassuring that person will not help over the long run. What we feed grows stronger.
It is advised that family members or close friends seek at least one session with a counselor who can help them understand what will be considered helpful.
Journal Articles: This webpage provides information on references and abstracts from MEDLINE/PubMed (National Library of Medicine).
OCD Statistics: Adults: This webpage lists information on the prevalence of OCD among adults.
Common Questions About OCD
Below are common questions which are random but frequently asked.
The short answer is YES they can. Even that one in your mind that you would rather not share with even yourself.
One major hurdle individuals have in getting treated is that they are scared or embarrassed to share their thoughts. Even as I share this with you, perhaps you’re thinking, yes but you’ve not heard “my” particular thought. Yes, that is true; however, there are a few things I hope I can help you understand:
- You’re not your thoughts. You’re not bad because you have any particular kind of thoughts or images passing through your mind.
- It would be right in line with what the OCD wants you to feel – afterall, who or what ‘wants’ to be annihilated? It will try to convince you that ‘maybe’ something will happen to you if you share with your therapist your deepest, darkest thoughts.
- As a therapist, the content of your thought does not make a difference in your treatment.
- I will not be calling the police or child services just because you told me you have certain fears or worries. I’m here to help you. But, if you don’t share I can’t help you don’t share, I can’t help.
- Everyone has the same kinds of thoughts. The only difference is we need to help your brain rewire the kind of responses it gives to those same kind of thoughts.
(Disclaimer: none of the information on this website is intended to diagnose or treat any condition. This information is for educational use only. Please get treatment if you feel you are struggling with different symptoms.)
Research shows that OCD does run in families and that genes play a role in the development of the disorder. Despite genes playing a role in causing the disorder, it is also believed that there is probably a combination of genetic susceptibility and environmental/social influences.
The reason for your developing OCD will be hard to identify, but it is believed that symptoms may have always been there or so subtle that the disorder was undetectable. Chances are there was a predisposition already present, then a stressor came along which triggered the symptoms you’re experiencing.
OCD can develop at any age, as early as preschool and continuing to adulthood. It tends to develop earlier in males: between athe ges of 6 and 15 years for males and between 20 and 29 for females.
There is no one explanation for why you developed OCD. Chances are
Sometimes when something stressful happens in a person’s life who already has a predisposition to OCD, the symptoms may worsen or become evident for the first time.
While we won’t know definitively why your symptoms may be appearing, the good news is that we don’t “need” to know in order to treat it. That “need” to know can sometimes become obsessive, and if so, we’ll surely know that upon assessment.
We cannot say that OCD is curable. There are times when your symptoms may not create distress for you or may not seem apparent at all, particularly due to treatment. However, you will need to learn how to effectively deal with times in your life when new or old obsessions start to become an issue for you.
People who are prone to have anxiety tend to struggle with it throughout their lives. There is no cure for anxiety, but one can learn effective means of coping and solving related issues.
Additionally, reducing stressors and taking care of your basic needs like eating a balanced diet, exercising, sleeping properly, and engaging in regular self-care, can mitigate triggers.
Disclaimer
None of the information on this website is intended to diagnose or treat any condition. This information is for educational use only. Please get treatment if you feel you are struggling with different symptoms.